Types of Immunity and Vaccinations (A-level Biology)
Types of Immunity and Vaccinations
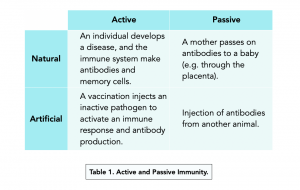
Natural and Artificial Immunity
Natural Immunity
- Natural immunity develops after infection. Natural immunity results from the body’s response to an antigen. When an organism is infected by a pathogen with a particular antigen for the first time, the body mounts a primary immune response which leads to the development of immunological memory.
- Memory cells are developed in the primary infection. During a secondary infection by the same pathogen with the same antigen, memory B cells and antibodies can quickly and effectively launch a secondary immune response to rapidly eliminate the pathogen
- Mothers can pass on natural immunity. Natural immunity can also be obtained by an infant from its mother. When babies breastfeed, antibodies can pass from the mother to the child through the breast milk.
Artificial Immunity (Vaccines)
- Artificial immunity is from vaccines. Artificial immunity results from the priming of the immune system through the use of vaccines.
- Vaccines are dead or weakened viruses. Vaccines are preparations of dead or weakened viruses which can be injected into an individual. These dead or weakened viral preparations have the necessary antigens in order to stimulate the immune system to develop immunological memory against the pathogen. This way, when an individual comes into contact with the live virus, the body already has an efficient mechanism in place to rapidly detect and eliminate it.
- Vaccines are currently only against viruses. It should be noted that currently vaccines are only designed against viruses.
Active and Passive Immunity
Active Immunity
Active immunity develops when the body makes its own antibodies in response to pathogen exposure.
- Vaccination provides active immunity. During vaccination, the immune system is actively geared to recognise and eliminate the particular pathogen. Active immunity is due to memory B cells and antibodies which are typically long lasting.
- Booster vaccinations may be needed. In some cases, with certain vaccines, an individual may need to obtain booster vaccinations after a period of time in order to revitalise the immunity. This is because for some vaccines, the immunological memory fades after a certain amount of time.
Passive Immunity
Passive immunity develops due to antibodies which come from another animal.
- Passive immunity is from injection of antibodies from another animal. In many cases, individuals infected by a particular pathogen need immediate treatment. One way of doing so is by injecting antibodies produced in an animal or antibodies from an immune person into the infected individual. Once injected, the antibodies can quickly identify the pathogen and help the infected individual’s immune system quickly fight off the infection.
Importance of Vaccination
- Our body can itself develop immunity. Upon infection, given enough time, our bodies can itself gain active immunity against a pathogen by developing an immune response. But this process takes usually takes two weeks.
- Many pathogens too quickly for our immune system. The process of mounting a successful primary immune response and gaining immunological memory usually takes around two weeks. Many pathogens, such as the Ebola virus, can kill an individual in a matter of days.
- Vaccines enable the immune response to occur quickly. Vaccination allows the body to be fully prepared to effectively combat pathogens. Data shows that vaccinations can allow the body to rapidly eliminate a live infection for the first time within seven days, with the peak of the immune response occurring within the first three days.
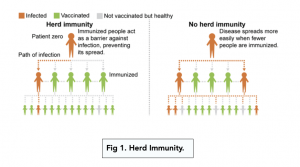
Herd Immunity
- Mass vaccination contributes to herd immunity. When the majority of a population is vaccinated against a pathogen, it breaks the pathogen’s chain of infection. This means that the virus essentially disappears because it is unable to pass from person to person. This means that members of the population, such as infants, who have not received vaccinations, are protected against the pathogen. This phenomenon is called herd immunity.
- Herd immunity is particularly important for infants. Many infants are too young to receive particular vaccines. Most vaccines are given to an individual over different stages of childhood to prevent certain risks. Therefore strong herd immunity is necessary in order to protect infants and other individuals who cannot be vaccinated for various reasons.
Ethics of Vaccination
Ethics of Herd Immunity
- Herd immunity can fall if people don’t get vaccines. If individuals in a population begin to lose their immunity by not vaccinating themselves or their children, it leads to a loss of herd immunity. Loss of herd immunity leads to a resurgence of disease.
- Near-eradicated diseases can return. Diseases such as whooping cough and MMR were almost eradicated due to vaccines. However, concerns over vaccinations lead to a big fall in vaccinations for these diseases. This led to a rapid resurgence of whooping cough and MMR, both of which can be fatal to infants and young children.
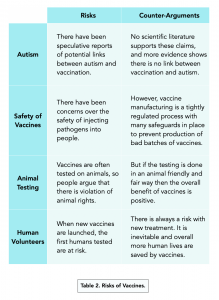
Risks of Vaccines
Antigenic Variability
- Vaccination relies on antigens staying the same. A vaccine stimulates the primary immune response, and produces memory cells against a specific antigen. It assumes that if there is a second infection, then the same antigen will be present on the pathogen.
- Sometimes antigens can change. Sometimes pathogens (especially viruses) evolve and alter their antigens, leading to antigenic variation. When these pathogens infect a second time, the memory cells are ineffective and a new primary immune response needs to be generated.
- Antigenic variation makes vaccination difficult. If the antigen changes, then the vaccine loses effectiveness.
Types of Antigen Variation
- Antigenic drift involves minor variations in antigenic structure, which can result in the production of new strains of a particular virus.
- Antigenic shift involves major variations in antigenic structure, usually leading to the development of entirely new types of viruses.
Influenza Virus Case Study
- The influenza virus evolves quickly. The influenza virus has a high rate of mutations, so new vaccines need to be developed every year to fight against new strains of the influenza virus.
- New strains can be present each year. Every year, there tends to be a new common strain which is present, therefore, an influenza virus is chosen each year based on the most common strain.
- Another issue is people not having the flu virus. Whilst the main problem is the antigen variability of influenza, another factor is the number of people who do not vaccinate themselves with the annual flu vaccine. Unvaccinated individuals readily catch the influenza virus, providing it with more opportunities to evolve and develop new strains, which further complicates the development of an influenza vaccine.
Evolutionary race between pathogens and host
Antigen variation is an example of how pathogens have evolved to evade their hosts’ immune mechanisms. Other examples of this are outlined below.
Tuberculosis
- TB is spread by respiratory droplets which gives them direct access to epithelial cells. TB is spread from one person to another by droplet inhalation. This means when the droplets are inhaled, the TB bacteria directly arrives at respiratory epithelial cells, which are its target site for infection.
- TB bacteria have a waxy, thick cell wall. This helps protect it against destruction by lysozymes.
- They can survive and lie dormant inside macrophages. Although they may be phagocytosed by macrophages, they are usually not completely destroyed due to their thick cell walls. This means that they can survive and lie dormant inside macrophages for a long period of time, and activate and reinfect the body at opportune times when the host immune system is weak.
HIV
- HIV has a high mutation rate. The antigens on HIV viruses can change rapidly, meaning that memory cells cannot recognise them and the body’s humoral immunity is ineffective.
- HIV targets helper T cells first. HIV targets and replicates inside helper T cells first at the beginning of its replication cycle, meaning the body’s normal immune response is disrupted and further spread of the virus cannot be stopped.
- HIV can lie dormant in the body for many years. The HIV virus can be dormant in the body for as long as ten years after the initial infection, thus, it can reactivate and cause illness without the person being infected from a new source.
Immunity refers to the ability of an organism to resist or fight off diseases or infections. It is the body’s natural defense mechanism against harmful pathogens.
There are two main types of immunity:
Innate Immunity: also known as non-specific immunity, it is the body’s first line of defense against pathogens and is present from birth.
Acquired Immunity: also known as specific immunity, it is immunity that is developed after exposure to a specific pathogen. It can occur naturally or through vaccination.
Active Immunity is immunity that is acquired through the production of antibodies in response to an infection or through vaccination. It is a long-lasting form of immunity that can last for several years or a lifetime.
Passive Immunity is immunity that is acquired through the transfer of antibodies from one individual to another, such as from a mother to her baby during pregnancy. It is a short-lived form of immunity and typically lasts for a few months.
A vaccination is a medical procedure that involves administering a weakened or dead form of a pathogen or a piece of the pathogen to a person, in order to trigger the production of antibodies. This helps to protect the individual against future infections from the same pathogen.
Vaccinations work by tricking the body into thinking that it is being infected by a real pathogen, which triggers the production of antibodies. The antibodies produced in response to the vaccination protect the individual against future infections from the same pathogen.
Vaccination provides several benefits, including:
Protection against diseases and infections.
Reduction of the spread of diseases and infections within communities.
Prevention of outbreaks and epidemics.
Protection of vulnerable populations, such as young children, elderly individuals, and those with weakened immune systems.
Like any medical procedure, vaccination may cause side effects, although these are usually mild and short-lived. Serious side effects are rare, but they can occur in some cases. It is important to discuss any concerns or questions about vaccinations with a healthcare provider.






Still got a question? Leave a comment
Leave a comment